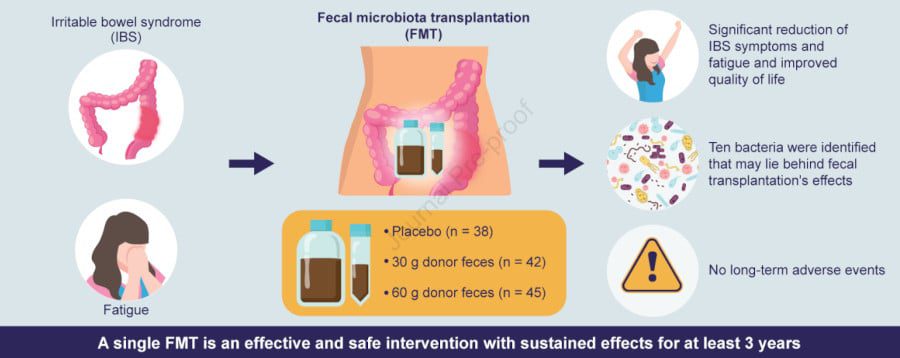
Approximately 11% of the world’s population suffers from irritable bowel syndrome, which is a very debilitating disease on a daily basis. This syndrome may result from an imbalance of the intestinal microflora, which may lead to a change in intestinal permeability and inflammatory reactions. Therefore, fecal transplantation has emerged as a potential treatment. A new clinical trial today confirms that this approach is effective, including in the long term.
Irritable bowel syndrome (IBS), also called “functional colonopathy,” is a benign disease, but it can seriously affect quality of life. Chronic abdominal pain, transit disturbances (alternating constipation and diarrhea) and other extra-GI symptoms (headache, fatigue, muscle aches, etc.) permeate the daily life of patients. Since the origin of this syndrome is still poorly understood, there is currently no treatment to treat it.
However, studies have revealed that the microbiome of people with IBS is out of balance: “bad” bacteria are in excess (we’re talking about “intestinal dysbacteriosis”). Refilling the intestines with a healthy mix of bacteria, via stool culture, can help restore balance and reduce symptoms of disease. A team from Stord Hospital in Norway set out to test this approach in a clinical trial that began three years ago: nearly two-thirds of the trial participants now report a better quality of life.
At least 77% of patients are relieved after three months
Some previous clinical trials have shown that faecal cultures reduce IBS symptoms. However, the adverse effects of this transplant and its long-term effectiveness were not known until now; Especially since previous studies on this topic only included a maximum one-year follow-up. This is why a Norwegian team performed a longer follow-up, over three years, in a randomized, placebo-controlled trial.
The experiment started in 2019. Dr. Magdi Al-Salihi and colleagues at Stord Hospital collected the faeces of a 36-year-old man. This donor was a non-smoker, in good health, taking no medications, and had a BMI of 23.5 kg/m2. His mother confirmed that he was born vaginally, breastfed, and had only been treated with antibiotics three times in his life. He regularly took nutritional supplements rich in protein, vitamins, fiber and minerals. Its microbes were considered ideal for transplantation.
Stool samples from this donor were transferred to the small intestine of 87 patients with moderate to severe irritable bowel syndrome. Some received 30g of stool, others received 60g, and 38 patients received their stool transplant as a placebo. None of the participants knew what type of stool was passed on to them.
After three months, 76.9% and 89.1% of transplant patients with 30 g and 60 g of donor faeces, respectively, reported reduced symptoms, regardless of disease severity. who received a placebo). These same patients also reported significant improvement in fatigue and quality of life. Only mild gastrointestinal symptoms were reported as adverse effects, but they resolved spontaneously. Three years after transplantThe results are equally encouraging.
Symptoms continued to decrease after three years, in at least 65% of participants
Study participants were asked about their health status after two years and then three years after faecal culture. ” Response rates were 26.3%, 69.1%, and 77.8% in the placebo groups, 30 g and 60 g, respectively, 2 years after transplant, and 27.0%, 64.9%, and 71.8%, respectively, 3 years after transplant. ‘, the researchers report in the journal Gastrointestinal Diseases.
So the improvement in symptoms was significantly greater in the groups that received donor stool than in the placebo group. These patients had less IBS symptoms and fatigue, and had better quality of life 2 and 3 years after transplant. The dysbiosis index (which reflects an imbalance of microorganisms) decreased only in the two groups who benefited from the treatment. By comparing the microbiota of different groups of patients, the team was able to identify 10 bacteria that had significant associations with IBS symptoms and fatigue. No long-term adverse events were recorded.
Dr. Al-Sahli explains in an interview That people with severe IBS responded better to treatment than those with moderate symptoms and that women also responded better to transplantation than men. In addition, ten patients (5 receiving 30 g and 5 receiving 60 g stool) who relapsed three years after a new transplant (90 g): most (80%) again showed early signs of improvement Three months.
If this study proves that this method is effective and provides lasting relief, it is unfortunately not generalizable due to the costs involved. Scientists hope to one day be able to isolate the beneficial bacteria from healthy donors in order to give them to patients in pill form.
source : M. El Salhy et al., Gastroenterology

“Subtly charming problem solver. Extreme tv enthusiast. Web scholar. Evil beer expert. Music nerd. Food junkie.”