published
Scientists from UNIGE found that the size of the intestine changes depending on the amount of food eaten. This is via a protein that can be inactivated.

The more we eat, the more our intestines change to absorb calories more efficiently. The process is however reversible.
Getty Images / istockphoto
Obesity is primarily the result of an imbalance between energy expenditure and calorie absorption. If you don’t burn it enough, you will gain weight. 40% of the world’s population is overweight and more than 10% is obese. Thus, one way to understand how humans grow is through the intestines.
This is where food that has been previously broken down before passing into the bloodstream is absorbed to be distributed throughout the body. And to absorb enough calories, the intestinal wall is covered in millions of convolutions called villi and microvilli, which will, eventually, cover the surface of the football field, the University of Geneva explains in a press release.
Amazing Intestinal Plasticity
“A few years ago, we discovered that the intestines can be lengthened or shortened depending on environmental factors and physiological needs,” recalls Mirko Trajkowski, professor in the Department of Cell Physiology and Metabolism and at the Diabetes Center. From UNIGE Medical School. Exposure to cold, for example, could be one of those external stimuli that changed the length of the intestines.
But how does this intestinal plasticity work? Using mice and 3D models of the human intestine, the researchers found that the food eaten is the main factor in changing the size of the intestine. “We observed a relatively rapid and physiologically impressive response to increased food intake: the intestine subsequently lengthened by more than 30% and was associated with a significant growth in the size of the villi and microvilli.” , explains Mirko Trajkowski, lead author of the study published Dec “Nature Communication”. The fact that these villi also grow larger, as can be seen below, made it possible to absorb calories more efficiently.
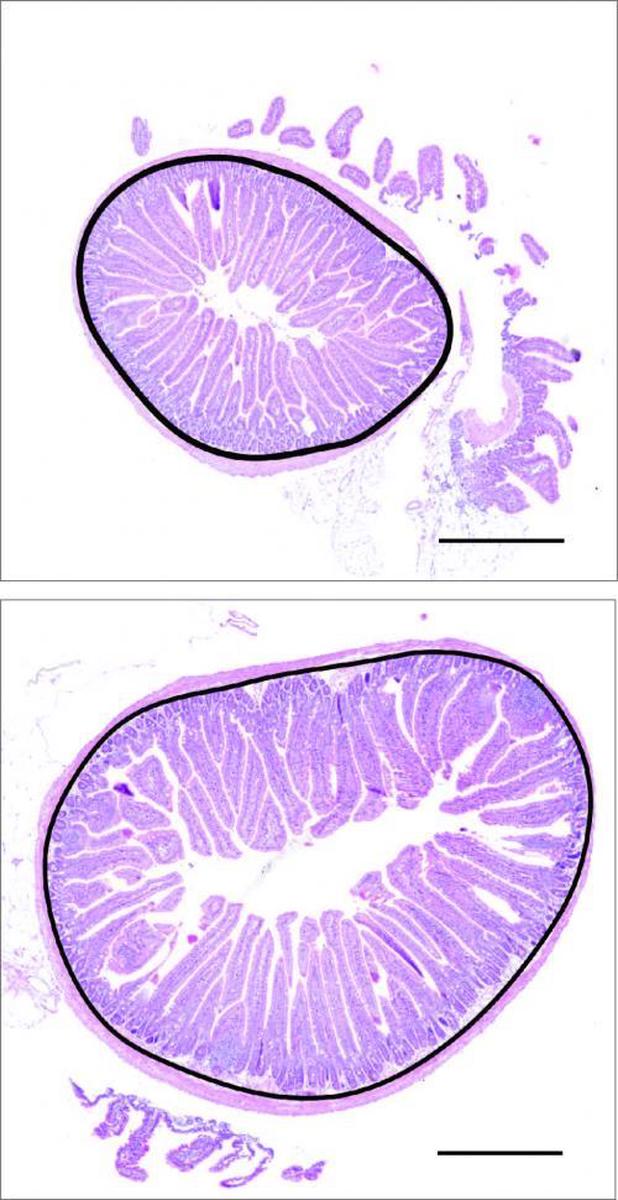
Sections of mouse intestine. Above, normal intestinal circumference (in black) and villi (in pink). Below, the intestine is enlarged after overeating with obesity, with a larger circumference and longer villi.
Mirko Trajkovsky
What is also interesting is that the process is reversible. If less food is eaten, the length and shape of the intestines return to almost normal. The scientists also found that increased intestinal absorption surface area drives various mechanisms that allow cells to convert food into energy. One of them, called the PPARα pathway, has proven to be absolutely essential. Indeed, the PPARα protein appears to control both the increase in villi length and caloric absorption capacity. It raises the level of another protein called PLIN2, which, by promoting the formation of fat droplets in the cells of the intestine, facilitates the absorption of fats.
Reducing the ability of the intestine to absorb
This mechanism can be confirmed by inactivation of PPARα in the gut of mice. Mirko Trajkowski notes that “its pharmacological inhibition did indeed lead to a marked decrease in the intestinal absorption capacity and also made it possible to reverse the fat accumulation and obesity caused by a high-calorie diet.”
Therefore this could constitute an interesting alternative to gastric bypass (surgery consisting of reducing the size of the stomach and modifying the nutritional circuit) or to other irreversible interventions aimed at reducing weight gain and obesity-related complications. But making PPARα inactive can be difficult. This protein “plays a key role in many metabolic functions, and is expressed in many tissues. Before presenting our findings to patients, we will therefore have to find a way to inhibit it only in the intestine without affecting other organs.” However, this is still a serious and promising line of research.

“Subtly charming problem solver. Extreme tv enthusiast. Web scholar. Evil beer expert. Music nerd. Food junkie.”