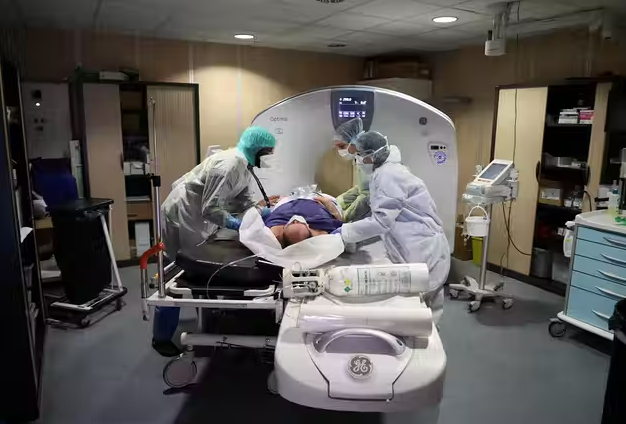
A patient infected with Covid-19 virus is about to undergo a CT scan.
©Ludovic Marin / Agence France-Presse
nervous effect
British researchers have studied the consequences of severe forms of Covid on the brain. According to this study from the University of Cambridge, persistent cognitive deficits were found, resulting in an effect similar to aging from 50 to 70 years old.
Atlantico: one A British study analyzed the consequences of the severe Covid virus on the brain. r . was foundThe results indicate persistent cognitive deficits. What would the tangible consequences be, according to this study?
Andrei Neulon: Yes, the study by the Cambridge University team confirms, following the study by the Oxford University team a few weeks ago, that a large proportion of people who have experienced a severe form of COVID-19, especially those who are hospitalized, have detectable cognitive deficits after More than 6 months after injury. In the Cambridge University study, the number of patients admitted to hospital with these cognitive impairments was at least about 30%. Studies show that cognitive deficits primarily lead to complex clinical pictures including generalized fatigue, a form of apathy that reflects loss of motivation, difficulty concentrating, sleep disturbances, generalized anxiety, or even a form of post-traumatic stress. More specifically, a form of mental confusion, with difficulty “finding words”, so-called “short-term” memory disturbances (instant memory), dizziness and inability to concentrate, presents a rather specific clinic picture of this type of infection, which It was actually suggested by psychiatrists at the University of Toronto a few months ago.
Read also
COVID-19: Virus could increase the number of cases of dementia and other neurological disorders for decades
Although in-hospital patients and especially those with the most severe forms requiring mechanical ventilation appear to be among the most affected by these long-term cognitive effects (30 to 45% of patients according to certain studies), it turns out that these effects are not limited to On these patients, but this deficit, and certainly less significant, can also be perceived in about 15% of people affected by COVID-19, including a form that did not result in specific hospital care, and even to 25% according to an American study. In general, the cognitive and mental damage is certainly greater than what has been measured in the general population to date.
What could explain in Covid an effect identical to aging between 50 and 70 years as suggested by the Cambridge University study?
In fact, the permanent decline in cognitive performance has been compared to the “normal” physiological aging process, with the exception of dementia, which, according to some studies, has led, according to some studies, to a decline in cognitive ability with age, which occurred more in the last decades of life, schematically after 60 General, though many debates qualify for this assertion. In any case, the cognitive impairment observed in patients who have experienced severe forms of COVID-19 has been linked, in particular by researchers at Oxford University, beyond the expected changes in olfactory-related regions, to a form of reductionism. In the cerebral, limited but highly realistic volume, of the brain regions involved in cognitive functions and especially the structures involved in the memorization process. Specifically, this brain imaging work shows a reduction in the so-called “gray matter” areas, that is, those containing neurons, by 0.2% and even 2% within a few months after illness, which is very important. This, moreover, is the main argument made by the Cambridge teams for suggesting that the effects of COVID-19 on the brain equate to premature aging because, physiologically, in the context of “normal” rather than pathological aging, the thicknesses of these same brain regions involved in conservation decrease ( the hippocampus in particular) ranges from 0.2 to 0.3% per year after 60 years. Therefore, the most significant reductions observed in these imaging studies are indeed associated with an age of at least a decade, as suggested by the study cited in ref.
Read also
Brain discovery explains why humans continue to grow and reach adulthood
The mechanisms of these brain alterations are less clear, and traditionally, the most common causes are associated with the effects of COVID-19 on the brain: exacerbated inflammatory processes that can lead to encephalitis, the body’s immune response to a dangerous condition likely to amplify encephalitis, and reduction in cerebral oxygenation during the acute phase. of disease is likely to enhance local discrete strokes (a number of studies have shown an effect of COVID-19 on the incidence of ischemic stroke), regardless of the direct effect of virus infection. However, at this point, nothing is certain, but the course of inflammation remains the most likely.
To what extent should these results qualify?
If the relationship between this brain damage and COVID-19 is undeniable, the fact remains that in other infectious diseases and especially in inflammatory damage of different origins, similar damage is observed and also produces similar behavioral effects. It is therefore possible that the clinical picture resulting from infection with COVID-19 does not present any particular specificity but reflects a non-specific cerebral response, in particular to the inflammatory process.
Moreover, as she points out, there is no consensus on the decline in cognitive abilities and mental health associated with aging, as some studies have not found age-related reduction in brain volume, or impairment of cognitive abilities outside of pathology. And even, in some studies, there is an improvement in verbal and arithmetic skills, perhaps in connection with the experience gained with age … So it is necessary to be careful with generalizations that may be offensive.
Read also
This is how the human brain develops from 0 to 100 years. What have we learned about innate and acquired?
What could be the long-term consequences of these severe Covid brain effects?
A number of concerns have been expressed about a possible increase in the incidence of neurodegenerative diseases in populations affected by the coronavirus pandemic. These speculative considerations are mainly based on the observation that as a result of the Spanish flu epidemic at the beginning of the last century, an increased incidence of these neurodegenerative diseases, especially Parkinson’s disease, was observed. Thus, certain teams have put forward the hypothesis that a group of patients who have experienced a (severe) form of COVID-19 may develop one or more of the more common neurodegenerative diseases, a form of Alzheimer’s disease or Parkinson’s disease. At this point, there is no indication that this may actually be the case among the millions of people who have been infected. But wisdom dictates that we reassure the population and advance that the worst is not the caseNever sure!

“Subtly charming problem solver. Extreme tv enthusiast. Web scholar. Evil beer expert. Music nerd. Food junkie.”